Interview
What comes after Omicron?
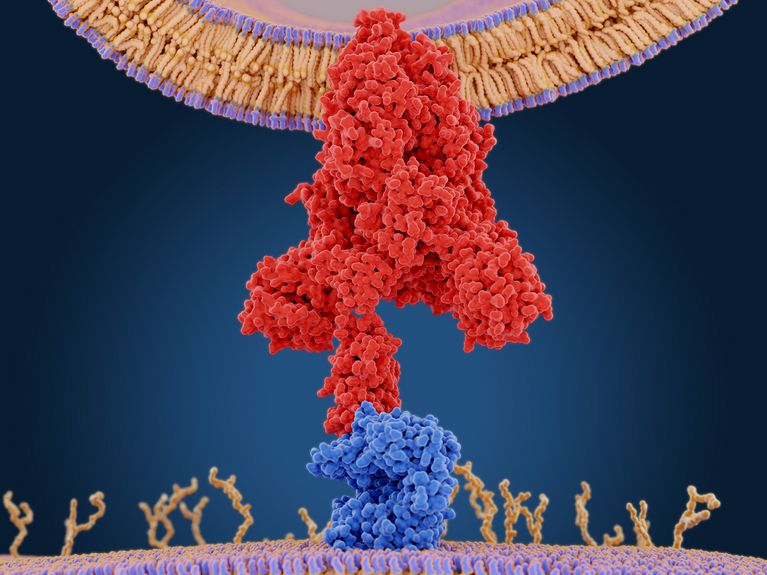
The coronavirus spike protein (red) allows the virus to enter the human cell by binding to the ACE2 receptor (blue). (Credit: Juan Gaertner/Shutterstock)
Luka Cicin-Sain from the Helmholtz Centre for Infection Research explains why Omicron is possibly a game changer, which variants we can expect in the future, and what we can do about them.
Mr. Cicin-Sain, the infection figures have been enormously high for weeks; does that at least equip us a little for the future? At least those who have been infected are protected for a certain time.
Unfortunately, according to current knowledge, a past Omicron infection only protects against other variants to a very limited extent, and this also applies in terms of time. There are studies with antibody neutralization tests. These are studies that test how well the antibodies found actually react to certain SARS-CoV-2 pathogens. This showed that the antibodies acquired through an Omicron infection do not work very well against the Delta variant. This suggests that the variants are very different after all.
Where are these differences? After all, it is still a Sars-CoV-2 virus. Aren't the basic structures the same?
The basic structures are the same, but in detail there are some differences in very different parts of the virus. Omicron, for example, seems to be more flexible in terms of docking sites. As is often the case, the focus is on the spike protein, which makes up the largest part of the virus: If you look at the coronavirus under the electron microscope, it has a kind of crown, hence the name. This crown is the spike proteins.
Is it the protein that allows the virus to enter the human cell?
Luka Cicin-Sain is an infection researcher at the Helmholtz Centre for Infection Research in Braunschweig, where he heads the Viral Immunology Group. (Credit: HZI/jab)
Correct. In order for the spike protein to infect cells, it attaches to specific surface proteins of the cell. Primarily to the so-called ACE2 receptor. But it also requires other proteins on the cell surface. An important one is a protease called TMRPSS2. This is particularly abundant on lung cells. We have evidence that Omicron can also target other proteases than TMPRSS2. On the one hand, this explains why Omicron replicates less in the lungs, which also accounts for the milder courses. But it opens up entirely new possibilities for the variant, and possibly for other variants originating from here: Other human body cells are more likely to be infected. We already observe that gastrointestinal symptoms are more prevalent in Omicron, even if pulmonary symptoms are milder. However, we must continue to monitor the situation carefully before drawing definitive conclusions.
That would explain the differences in infectivity. And in terms of immune response? Can we expect new immune escape variants that can bypass the defense mechanisms of even an immune system trained by Omicron infection?
I think that is quite likely. The fact that it is heading in such a direction is in the nature of things: The virus is currently under increasing pressure due to the immunocompetence of the many vaccinated and recovered people. This selection pressure can lead to the spread of variants that have found a way through, like Omicron.
As you say, Omicron also has rather milder courses. Can we assume that this will also be the case in the future, with future variants? That's one hope, that the virus will become so harmless that it will eventually become endemic and not bother anyone....
That is a possibility, but it is far from certain. In a way, you have to look at the whole thing from the evolutionary-biological perspective of the virus: For the selection pressure on the virus, it doesn't make much difference whether it leads to a death rate of 0.5 percent, 1 percent or 2 percent. However, for the health of the population and for our health care system, these differences are significant. Therefore, we should not put too much faith in new variants necessarily being milder.
How can this high protective effect of the vaccination be explained? With a vaccination, only a part of the virus is vaccinated against, the spike protein, whereas with an Omicron infection, there are a lot of targets against which antibodies can be formed.
There are several reasons for this. First of all, the spike protein-as already mentioned-plays a key role in cell infection, and the antibodies that recognize it knock out the virus. Moreover, in a natural infection, the contact with the virus is not so intense: The virus is then often already recognized in the respiratory tract and controlled there, which leads to the formation of fewer antibodies because the antigen hardly reaches the lymph nodes and hardly stimulates lymphocytes. With a vaccination, on the other hand, the viral antigen enters the body unstoppably, so to speak, and the spike proteins are formed by the body's own cells and are channeled to the lymph nodes. The whole process is repeated at the second vaccination dose and at the booster; both the quantity and quality of the immune response increases. This naturally results in a more sustained immune response. By the way, this can also be seen in the comparison of the antibody titers of vaccinated and recovered persons.
Should we continue to vaccinate more and regularly in the future?
I don't think this is a solution because the response eventually exhausts itself, studies with a fourth vaccination already show that the effect offers only limited advantages over the third dose. A fourth vaccination is likely to be considered mainly for certain subgroups of the population at increased risk, such as the immunocompromised or the elderly. The situation would be different if we had a so-called polyvalent vaccine, in which case another vaccination across the population might be an option.
What are the advantages of a polyvalent vaccine?
A polyvalent vaccine basically contains many variants, and thus also offers broader protection. Such a vaccine is still being researched, and whether it will contain only Alpha, Beta, Delta and Omicron or other variants will also depend on how the virus mutates in the future. It is paradoxical and also elegant in terms of evolutionary biology: The better we get at research, the more effective our vaccines and remedies become, the greater the pressure on the virus becomes, and it changes more quickly and in a more targeted way, as it were. It's an exciting interplay. The virus is resourceful, but so are people.
Readers comments